Behavioral health urgent care hopes to fill critical need in Robeson County
Tulane University librarians sign to form a union; Novant Health aims to build hospital in Buncombe County; Proposed Public Media Cuts Will Hurt Rural Americans

It's Friday, July 18, 2025 and in this morning's issue we're covering: A new behavioral health urgent care hopes to fill an urgent need in Robeson County, Those in prison and their families and friends continue to deal with the high price of phone calls, Republicans cap student loan debt, Tulane librarians sign to form a union, Novant Health aims to build hospital in Buncombe County, Rate decision on hold as Wingate tracks down Siemens funds, Former jailhouse lawyer Calvin Duncan to run for Orleans Parish Clerk of Criminal District Court, Proposed Public Media Cuts Will Hurt Rural Americans.
Media outlets and others featured: Border Belt Independent, Bolts, CalMatters, Verite News, Asheville Watchdog, Mississippi Today, The Lens, The Daily Yonder.
Trillium to provide $2 million for the center, which is expected to open by the end of 2025
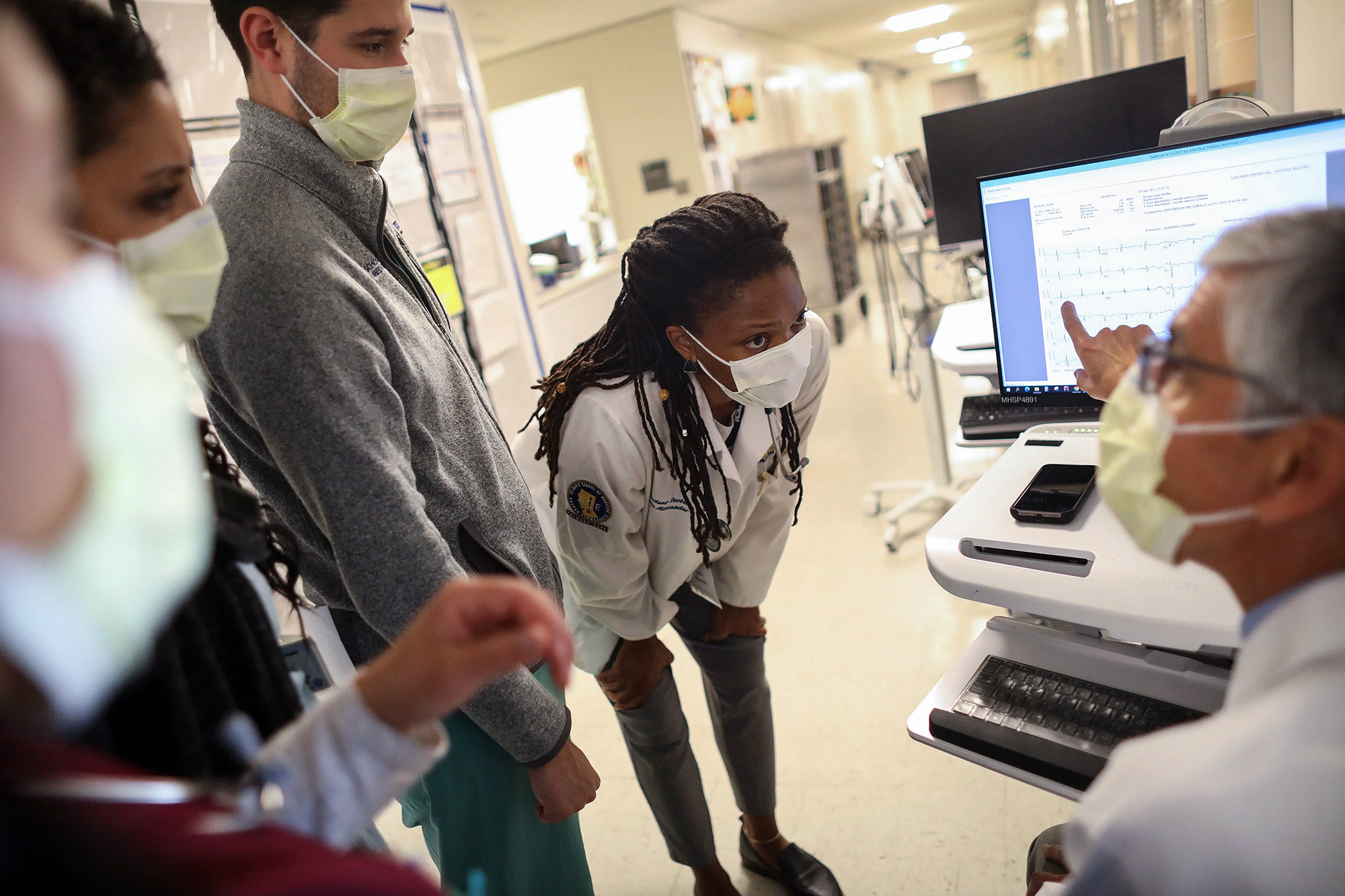
James Granger says primary care doctors shouldn’t just focus on patients’ physical health. Their mental well-being is just as important.
“Being able to do both, to understand both aspects, makes sense to us in being able to send that person on their journey,” said Granger, the chief operating officer for Southeastern Integrated Care. “It makes sense for the community here and rural areas that are underserved.”
Southeastern Integrated Care, which takes a holistic approach to medicine, will operate a 24-hour behavioral health urgent care center for adults and children in Robeson County. Trillium Health Resources, which manages mental health services in much of eastern North Carolina, is providing $2 million for the center, which is expected to open by the end of the year.
The goal of behavioral health urgent care centers is to keep people struggling with mental health issues—from panic attacks to drug misuse—out of hospitals’ emergency rooms that often have long wait times and lack the resources to provide a calming environment.
North Carolina has increasingly looked to behavioral health urgent care centers as a way to help people in immediate need. The state Department of Health and Human Services said in April 2024 it planned to invest about $15 million for nine centers in Alamance, Buncombe, Caldwell, Haywood, Onslow, Pitt, Rockingham, Rowan and Vance counties. The move would increase the state’s behavioral health urgent care services by nearly 50%, DHHS said.
The state health department and Trillium announced in January their plans to award more than $13 million to providers to open behavioral health urgent care centers and community crisis centers in Lenoir, New Hanover and Pitt counties.
A behavioral health urgent care respite facility for children opened in the Columbus County town of Chadbourn in June. The center can accommodate up to six young people with mental health issues for short-term stays to relieve families and caregivers.
In Robeson County, adults reported having poor mental health on 5.7 of the previous 30 days, according to the latest County Health Rankings from the University of Wisconsin Population Health Institute. That was higher than the statewide figure of 4.9 days, according to the rankings, which used data from 2022.
Robeson County residents said obesity, mental health and substance misuse were the top health issues that need to be addressed, according to the county’s 2023 Community Health Needs Assessment.
In 2023, 878 people in Robeson County sought help for depression at the emergency room, according to the state’s Mental Health Dashboard. More than 600 sought help for depression, and about 850 sought help for suicidal thoughts.
Granger said emergency rooms are crucial for treating life-threatening injuries or illness. But building relationships is key for behavioral health.
“That traditional emergency room model of care is not designed to adequately serve this vulnerable population,” he said.
Lori Dove, the senior vice president and chief operating officer at UNC Health Southeastern, Robeson County’s only hospital, said in a statement that a continued increase in patients seeking mental health care in the emergency room is an ongoing concern.
“The rise in visits underscores the need for more accessible mental health care options, including outpatient services and community support systems,” Dove said. “Through the implementation of integrated care models, where mental health professionals are part of the emergency care team, outcomes can be improved for all patients.”
Anthony Grimaldi, chief innovation officer at Southeastern Integrated Care, said in a statement that the new center “will provide the right place at the right time for the right client to receive psychiatric and substance use disorder stabilization services in a milieu environment that’s conducive to safety, wellness and recovery.”
Medical providers at the Pembroke office of Southeastern Integrated Care are already equipped to treat patients’ physical and mental health. The office provides individual, family and group therapy, along with medication management and community support teams. Many of the services are designed for patients with substance use disorders.
Trillium approached Southeastern Integrated Care about six months ago about operating a behavioral health urgent center, Granger said.
The facility will be at 105 Farmbrooke Drive in Lumberton, which currently houses the office’s Advanced Medical Home program. About 3,000 square feet of the building will be dedicated to the behavioral health unit, which can serve up to 12 patients a day, Grimaldi said.
Uninsured people will not be turned away if they can’t afford to pay, Grimaldi said, and the center will accept patients who have Medicaid. Along with serving patients experiencing mental health crises, the center will care for those with intellectual and developmental disabilities and traumatic brain injuries.
Southeastern Integrated Care plans to hire 15 to 20 additional staff members skilled in urgent behavioral health care for adults and children.
NC Child, a nonprofit that advocates for children’s well-being, gave the state an F grade for mental health in its 2025 report card. Adolescents ages 12 to 17 who had a major depressive episode increased nearly 27% between 2018-19 and 2022-23, according to the report.
Nearly 42% of Robeson County residents are Native American, as the county is home to the Lumbee tribe and many Tuscarora people. Since 2019, Native Americans have visited emergency rooms across the country for mental health issues at a higher rate than other racial group except white people, according to the Centers for Disease Control and Prevention.
“It makes sense for the community here, and especially in rural areas that are underserved,” Granger said. “I think it pushes for the community and overall health of its citizens.”
Sonya McGirt, a therapist in Lumberton, said expanding mental health services in Robeson County might encourage more people to seek counseling. It’s helpful when primary care doctors refer patients to mental health professionals.
“That’s a really common way people end up with a therapist: Someone or their doctor suggests it,” she said. “I’ve noticed that for a lot of people who either don’t trust therapy or don’t think to seek it out, they will sometimes have someone that ends up suggesting it. That’s why it’s helpful when doctors do it, because people should be seeing a doctor.”
Granger said the new center will add another option for people struggling with mental health issues.
“We’re just excited to see how the community responds to it,” he said.

Priced Out of Phone Calls Home
The FCC blocked Biden-era limits on the exorbitant rates and fees charged by prison telecom companies, leaving incarcerated people and their families to fight for state-level reforms.
Phillip Vance Smith II | July 10, 2025
Amber Nance learned of the crushing financial cost of keeping in contact with someone in prison after her husband was sentenced to serve seven years in North Carolina for a crime that she maintains he didn’t commit. “Right now I spend over $300 a month on the phone and video visits,” Nance told me in a recent call, estimating she’s spent around $20,000 total on calls from prison during the six years her husband has been inside—all so that he could continue fathering their three children while he served out his sentence. “I could have spent that on a down payment for a house,” she said.
The exorbitant price that Nance and millions of others pay to talk with family in prison has become a key organizing issue for advocates for incarcerated people, who have ramped up reform efforts in recent years to reduce or even eliminate fees that families pay to prison telecom companies. Activists have pushed several states and large counties to make phone calls free for incarcerated people, and in late 2022 Congress passed the Martha Wright-Reed Fair and Just Communications Act, which clarified the Federal Communications Commission’s statutory power to regulate in-state prison calls.
Last summer, the newly-empowered FCC voted to cap prison phone calls at 6 cents per minute and limit video call charges to 16 cents per minute. Starting this year, those new limits were set to kick in and lower costs across prison and jail systems in states that have resisted reforms, including North Carolina.
However, on June 30, Brendan Carr, who was tapped by President Donald Trump to chair the FCC, blocked those new rules from being enforced, issuing a two-year waiver for prison telecom providers to comply with the new caps and said the commission would “assess potential changes” to the new regulations. In a statement, Carr said the new limits—which started being enforced on a staggered basis across the country starting in January, and had been set to take effect in North Carolina the day after his announcement—were “leading to negative, unintended consequences,” such as some institutions planning to scale back phone services in reaction to the new caps on rates that can be charged.
FCC Commissioner Anna M. Gomez, who was appointed under President Joe Biden, issued a statement accusing Carr of stalling and ignoring both the law and the will of Congress in order to shield “a broken system that inflates costs and rewards kickbacks to correctional facilities.”
As a result of the FCC blocking the new rules, the rate that I and others who are incarcerated in North Carolina have to pay for phone calls will remain 10 cents per minute, rather than dropping to what was supposed to be the new federal limit of 6 cents per minute this summer.
These costs for communicating add up, and will continue to mostly fall on family and friends of incarcerated people. My job as a janitor inside Neuse Correctional Facility, a medium-custody prison in Goldsboro, earns me only about $7 a week. Since I can’t afford much on my own, the costs of keeping in touch often get passed on to loved ones like my mother, who has paid varying rates to talk with me over the course of my 23 years in prison. At one point, she has shelled out as much as $15 for a single 15-minute phone call.
Communication with the outside is vital for us. When the pressures of incarceration become too difficult to cope with on my own, my support system is only a phone call away. I’m fortunate that, even with the high cost of phone calls, my loved ones send money to help keep us in regular contact. My sentence of life without parole, coupled with the far distance it takes to travel to the prison and other restrictions on visitation here, means I will likely never physically spend time with many of my family and friends ever again. But through these phone calls, I can still rely on their emotional support and encouragement, even if they are just a voice hundreds of miles away. Without them, I would be lost.
Twenty-nine year old William Kohler isn’t so lucky. Kohler, who works as a janitor with me here at Neuse, told me he’s lost most of his family contacts since being sent to prison a decade ago, and says he gets no money from the outside to help with calls. To talk with his 12-year-old daughter, he relies on the free five-minute phone call that ViaPath, the telecom company that contracts with North Carolina’s prison system (formerly Global Tel Link, or GTL), has provided to all incarcerated people once a week. On weeks that Kohler needs to call a cousin or friend to deal with other matters, he has to skip the call with his daughter—meaning that sometimes they can’t speak at all for two or three weeks.
“Sometimes she’ll ask if I can call back,” Kohler told me as we spoke in a raucous day room at Neuse. “I ain’t got the money to afford it, but I feel like she thinks I don’t care about her when I don’t call back. Believe me, I wish I could call back to hear about her day or give her advice about life—you know, all the things a father should do. But I can’t.”
Kohler says he couldn’t afford more calls with family even if ViaPath lowered the rate to the cap of 6 cents per minute that the FCC set last summer. Paying for more calls, he says, would mean sacrificing hygiene or food items he needs to survive in prison.
A wave of activism by people directly impacted by the high price of communicating with loved ones behind bars—many of them mothers, children, and spouses of incarcerated people—has reduced costs for incarcerated families across the country in recent years while putting a harsher spotlight on the companies that reap massive profits off prison communications. Activists have so far pushed five states to make all prison phone calls free: Connecticut, California, Colorado, Minnesota, and Massachusetts. Several large U.S. cities also now provide free calls for people incarcerated inside local jails.
In North Carolina, a group of women with incarcerated loved ones last year formed a coalition called Connecting Families NC to lobby lawmakers for free phone calls in the state’s prisons.
Kristen Powers, one of the coalition members, is also the executive director of Benevolence Farm, a reentry nonprofit that provides housing and employment opportunities for women leaving prison in the state. Powers told me she’s witnessed women she works with struggling to stay in contact with incarcerated loved ones after release; she also told me about her personal experience paying exorbitant prices for phone calls to talk with a friend incarcerated in an immigration detention facility before he was deported.
“People in prisons and jails need to stay in touch with the outside to maintain family bonds,” Powers said. “The more people you have on your team when you get out, the better. We’re not meant to go through things alone. People come to Benevolence Farm because they’ve lost family connections. A hard transition back into society can be the consequence of those lost bonds.”
Powers’ coalition is pushing for legislation to make North Carolina the next state to make prison phone calls free, but the group has struggled to find a legislative sponsor in North Carolina’s General Assembly, which is led by the GOP. The draft legislation the group has circulated among activists and lawmakers would also prohibit state and local agencies from accepting so-called site commissions for prison telecom contracts—a practice in which the companies share a percentage of profits with the carceral system, which is a major factor in driving up high-cost, monopoly contracts for these services.
Read more:

Republicans cap student loan debt. Why that’s bad news for California medical students
By Mikhail Zinshteyn and Kristen Hwang, CalMatters
This story was originally published by CalMatters. Sign up for their newsletters.
Becoming a doctor will likely become even more difficult under the new tax bill Congress approved after lawmakers slashed the amount of money medical school students can borrow in federal loans.
The extra burden may mean fewer students choose careers in medicine, particularly low-income students. Patients, in turn, may see fewer doctors practicing family medicine.
The new rules, part of the sweeping Republican-backed “big, beautiful bill” that President Donald Trump signed into law July 4, cap federal debt for professional degree students at $50,000 annually and $257,000 for the life of a student’s college journey, including undergraduate debt.
Previously graduate students could borrow up to the cost of their programs to afford their degrees with so-called Grad PLUS loans. Starting next year, those loans will disappear. While all graduate programs are affected by the new law, medical school lasts four years and regularly requires more than $300,000 for tuition, housing, food and other expenses for a degree.
Without public loans, many students will have to borrow from private lenders, which provide far fewer protections for loan repayment and, unlike federal plans, don’t offer loan forgiveness.
Public service loan forgiveness, which can occur after 10 years of employment in nonprofit settings, is a particular draw for medical school graduates who choose to work in government or nonprofit hospitals and care facilities that pay less but have a mission of treating the poor.
Private lenders may also deny some students loans or charge higher interest rates based on their financial history. Private loans typically require cosigners, which not all borrowers are able to arrange.
Martha Santana-Chin, chief executive of the insurer L.A. Care Health Plan, said the cost of college, medical school and loan repayment already presents “financial barrier after financial barrier” that prevents many from pursuing medicine. Reliance on private loans will make it even harder for low-income students in particular to become doctors, she said.
“If you don't have access to loans, if you don't have access to preferred loan terms, it's going to be that much more difficult for you,” Santana-Chin said.
The lower borrowing limits are a key way Congress tried to record savings in the tax bill. By capping how much graduate students can borrow, limiting how much loan debt is forgiven and increasing in many cases how much borrowers of all degrees pay monthly, taxpayers cover less of the tab. But the Republican bill includes huge tax and revenue cuts that, even with other budget savings, add more than $3 trillion to the national debt in the next decade. The higher-ed savings were about $300 billion.
”Straightforward economic logic would suggest (the new rules) are going to make it less likely for some of those students to be able to pursue graduate degrees than they are now,” said Jordan Matsudaira, a professor at American University. He was also chief economist at the U.S. Department of Education during the Biden administration.
“I don't think we've ever been in a position where we've sent students to the private loan market looking for loans on this scale to be able to finance their education,” he added.
California medical school debt levels
U.S. Department of Education data from the Biden administration that Matsudaira shared with CalMatters show California’s largest producer of doctors, the University of California, regularly graduates students with debt in excess of $200,000, the most the new law says a graduate student in a professional program may borrow from the government.
- At UC Irvine’s school of medicine, the median debt from federal loans for med students was $195,000 for the years 2019-20 to 2022-23. That means that half of the students borrowed more and likely almost all of the new students in those situations would need private loans. Twenty-five percent of students there borrowed at least $254,000 and 10% borrowed at least $284,000.
- Every UC medical school had at least 10% of graduates with debt above $200,000. For UC Riverside, it was $270,000. At UCLA and UC San Diego, 10% of graduates borrowed more than $255,000.
- Many new graduates in similar situations would need $55,000 to $70,000 or more in private debt to finance their education.
- Four of the six UC medical schools had at least 10% of students borrowing more than $73,000 in a single year; new students in similar situations would need to find at least $23,000 in financing from private loans or some other support.
- At the private University of Southern California, 50% of graduates borrowed more than $260,000, and 25% borrowed in excess of $328,000, so a large chunk of new students would need to borrow at least $128,000 in private loans or find other ways of paying. A spokesperson for the school said no one was available to answer CalMatters’ questions.
There were 1,334 students graduating with medical degrees and 361 with similar doctor of osteopathic medicine degrees in 2023, a UC San Francisco report found. The UCs accounted for nearly 800 medical degree graduates.
The University of California perspective
Calvin Yang, a rising senior at UC Berkeley, said attending medical school has been his dream since he was a child. The new caps on federal borrowing won’t deter him from becoming a doctor, but they’ll slow him down and may force him to attend cheaper schools.
He plans to take at least one gap year after he graduates next spring and work to save as much as he can to avoid private loans.
“It's frustrating to see restrictions on our ability to simply want to pursue an education in order to help the world, right?” he asked. “Long COVID persists. Mental health remains a major issue, diabetes, obesity — those all require medical professionals.”
He thinks some students will “reconsider the medical school pathway.” The loan caps are a concern among his friends with medical school ambitions.
“We do think that the private market will meet a lot of the needs of those students,” said Shawn Brick, associate vice provost of student financial support for the UC Office of the President. “Approval rates are fairly high for medical students.”
Still, “we do share the concern … about the student who may not have credit that would give them access to loans in the private market.”
Brick said the UC has time to work with private lenders on financial products that “would be more accessible to students who maybe don't have the best credit.”
The median loan size UC med students have had to borrow has declined by about $50,000 over the past four years, adjusted for inflation, UC data show. At the same time, UC grant aid for med students has grown by about 50%.
Nearly 3,000 UC med students receive an average of $32,000 in UC grants to support their education. The UC also issues its own loans, but in small numbers.
Doctors and advocates weigh in
Even before these changes, Dr. Julián Restrepo said medical school leaves doctors with so much debt that he knows people who are paying off loans decades after graduating, surgeons who work multiple jobs and resident physicians who pick up extra shifts to make ends meet.
“It is a huge burden for us, and it very well determines where we live, where we work, how we work and how we manage our practices,” Restrepo said.
Restrepo graduated from Texas A&M University’s medical school in 2012 and did his residency at Los Angeles County Medical Center. He now works as a primary care physician at a federally qualified health center in Los Angeles and said public service loan forgiveness is an effective way to recruit high quality physicians and specialists to underserved areas.
With interest, Restrepo’s loan of about $230,000 grew to more than $300,000. He made payments on the loan as part of the public service loan forgiveness program for about seven years until a Biden-era loan forbearance program temporarily kicked in.
An L.A. Care program aimed at recruiting physicians to underserved areas will pay off the remainder of his loans, and Restrepo said he’s extremely fortunate. At many points in his career he was forced to defer his loan payments because he couldn’t afford it.
The Association of American Medical Colleges also thinks the impending reliance on private loans may lead to fewer future doctors. “We are concerned that this added barrier could deter qualified candidates from pursuing a medical degree altogether, which could ultimately worsen the existing and expected physician workforce shortage,” said Kristen Earle, director of student financial services at the association, which oversees the medical school entrance exam. The association projects a national shortage of 86,000 physicians by 2036. California, like much of the country, has a shortage of primary care physicians, with the Central Coast, Central Valley and Southern Border regions projected to have the most severe shortages.
More pressure on medical residents
And while medical degrees eventually lead to relatively high salaries that are typically $220,000 a year to more than $400,000 depending on the specialization, early career doctors earn much less in residency, a training period of three to sometimes seven or more years. As residents, doctors work 60 to 80 hours a week for salaries of about $70,000 to $100,000, depending on the region and whether residents are unionized.
Private lenders offer a wide range of interest rates for medical school, from about 3% to more than 14%. Federal rates fall in the middle of that range, are less variable and pegged to inflation. Some private lenders indicate online that they don’t require borrowers to pay while they’re in residency for a few years, while others require only a small payment. In either case, the unpaid interest grows the overall debt a borrower will have to pay off.
Earle said she hopes that private lenders keep interest rates fairly low for medical school students because they're a good bet to pay off their debt given the higher earnings potential.
Dr. Mahima Iyengar is in her final year of residency at the massive Los Angeles General Medical Center to become a primary care physician.
She said she borrowed $250,000 in federal loans to attend medical school — $50,000 above next year’s maximum — and has no idea how someone like her would have avoided private loans. She wanted to study at the public University of Maryland, a less expensive option in her home state, but wasn’t admitted. Instead she attended the University of Rochester, another highly competitive but pricier private medical school hundreds of miles from home.
“I could have tried to live cheaper in med school, but I don't think it would have been much more possible than how I was living with three, four roommates,” said the 31-year-old, who’s also a leader in her union.
Like a majority of medical school students, Iyengar knew she’d use public service loan forgiveness.
Now that option will be gone for professional school debt above $200,000.
“We want a diverse group of people taking care of patients, because we know that patients have better outcomes from providers that understand where they've come from,” she said. But that diversity might ebb if lower-income students, who are more likely to be students of color, feel priced out of med school.
UC agrees. “We don't know for sure, but we are concerned about this slowing the efforts to build the physician workforce across the country, and especially in California, where we've got significant needs in primary care in rural areas,” said Heather Harper, spokesperson for UC’s medical operations.
L.A. Care has invested $255 million since 2018 in scholarships for medical students and loan repayment for physicians to try and recruit doctors, but Santana-Chin said it’s not enough money to meet the need. She hopes that medical schools see the federal changes as a “call to action” to make education more affordable, she said.
This article was originally published on CalMatters and was republished under the Creative Commons Attribution-NonCommercial-NoDerivatives license.
Tulane librarians sign on to form a union, petition for formal election
by Safura Syed, Verite News New Orleans
July 11, 2025
Librarians at Tulane University announced the formation of the Tulane Workers United Librarians Union last week (July 3), after 87% of eligible librarians signed cards in support of unionization. Through the bargaining process, librarians hope to codify their roles on campus and create foundations for sustainable and long-term careers at Tulane.
University librarians acquire resources, connect students with resources, run independent catalogues, teach and help professors with research — all while publishing research of their own. Adi Flory, who works in Tulane’s Law Library, said the services that Tulane’s librarians provide allow the university to maintain its status as a premier research institution. Still, Flory said her current salary of $60,000 is barely enough to cover her mortgage and debts from her postgraduate studies. Law librarians are required to have both law school and library science degrees.
“As far as academic law librarians go, our pay is not competitive in any way,” Flory said. “By the end of the last week of the month, I don't have much left in my bank account.”
Katherine Hicks, a scholarly engagement librarian at Tulane’s main library, said that librarians are often overlooked on campus. Most Tulane employees fall under one of two categories: faculty, which includes professors and lecturers; and staff, such as janitors, cafeteria workers and groundskeepers. But librarians don’t fall neatly into either group. Like staff, librarians have regular working hours, but they also perform the duties of teaching, publishing and researching commonly associated with faculty members. The unique role requires a different handbook, Hicks said, but one hadn’t been reviewed since the 1980s. Last year, librarians came together to revise the handbook.
As librarians worked on the handbook, ideas about unionization also started to form. Hicks said she and a small group of librarians began talking about unionizing last year, with discussion expanding slowly until this summer.
Hicks said the percentage of librarians who signed on to the union jumped from 20% to 87% in just three weeks, right before the union went public. She said it felt “surprisingly amazing,” to see her colleagues' interest in collective organizing.
“No one is angry at the administration, no one is having specific issues,” Hicks said. “A lot of it is about us. It's not about the administration. It's about us wanting to have a platform for defining our role and our job.”
Although the union hasn’t yet defined its bargaining goals, Flory said she hopes a new contract would enshrine benefits, create a transparent and standardized promotion structure and leave librarians time in their work hours to perform and publish their research.
The librarians are organizing under Workers United, an affiliate of the Service Employees International Union, which submitted a petition for formal election with the National Labor Relations Board on July 7. Hicks said they hope to receive an election date by July 16.
Last year, non-tenure track faculty across five schools at Tulane voted to unionize with Workers United and are involved in ongoing contract negotiations with administration. Hicks said that vote was a “big boost” to the librarians’ organization efforts. She said the existence of another union on campus helped people feel more comfortable in signing on.
Hicks and Flory said the union hasn’t yet received a formal acknowledgment from Tulane administration, which has the option to voluntarily recognize it and avoid an election.
“Tulane fully supports the rights of employees to vote on whether they want to be part of a union or not,” said Tulane spokesperson Michael Strecker in an email to Verite News.
Safura Syed is a Report for America corps member who writes about education for Verite News.

This article first appeared on Verite News New Orleans and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.

Novant Health aims to build hospital in Buncombe County
Nonprofit will compete with AdventHealth for approval through state’s Certificate of Need process
by ANDREW R. JONES July 11, 2025
Novant Health will seek permission from the state to build a hospital in Buncombe County, competing with AdventHealth for 129 acute-care beds, Asheville Watchdog has learned.
“Over the past year, we’ve worked closely with the community and local physicians to grow our specialty care network in the region and look forward to applying in October for the additional beds outlined by the State Medical Facilities Plan (SMFP),” a spokesperson for the Winston-Salem-based nonprofit healthcare company told The Watchdog. “We will share more details about the proposed hospital soon and will continue to provide updates at NovantHealth.org/WesternNC.”
Buncombe, Graham, Madison and Yancey counties need 129 acute-care beds, according to the 2025 SMFP. Novant will apply for those through the state’s Certificate of Need (CON) system, which subjects medical expansions to a competitive process.
Novant already faces competition for the beds.
Florida-based AdventHealth recently announced its intent to acquire them and expand its already-approved 93-bed hospital in Weaverville to 222 beds, which would make the facility the region’s second-largest behind Mission Hospital in Asheville.
Mission Health is the largest hospital system in western North Carolina, with its six hospitals containing a total of nearly 900 acute-care beds, including 682 in Asheville. Mission Health did not respond to a question about whether the HCA Healthcare-owned system would apply for the beds, but it has routinely sought beds when they have become available through the CON process.
In 2022, Mission, AdventHealth and Novant competed for 67 acute-care beds and again in 2024 for 26 more. AdventHealth won both those CON applications.
Mission appealed both decisions in court, but lost in its bid for the 67 beds. AdventHealth and Mission are awaiting a final decision from the state’s Office of Administrative Hearings on the 26 beds. Novant contested the awarding of 67 beds to AdventHealth but dropped its court case in early 2023.
Healthcare companies can apply for the 129 beds on October 15.
The SMFP is a document annually published by the North Carolina Department of Health and Human Services. Staff analyze state population and hospital patient data, using a complex methodology to come up with a “determination of need” each year.
The draft version of the 2026 SMFP lists a need for 92 beds, meaning health systems that don’t win the 129 beds may have another opportunity to expand next year.
Novant has been trying to establish a presence in the area for years; it attempted to buy the Mission Health system before HCA Healthcare sealed that deal for $1.5 billion in 2019.
In late March, Novant lost a CON bid to build a diagnostic center at the former Gold’s Gym site on Hendersonville Road in Asheville. But it’s established at least seven clinics in the area since 2023:
- Novant Health Asheville Endocrinology
- Novant Health Women’s Specialty Care in Asheville
- Novant Health Plastic & Reconstructive Surgery in Biltmore Park
- Novant Health Surgical Partners in South Asheville
- Three GoHealth urgent care locations in Asheville and Black Mountain
Novant Health has nearly 900 locations, including 19 hospitals, more than 750 physician clinics and urgent care centers, outpatient facilities, and imaging and pharmacy services, mostly in North Carolina.

Rate decision on hold as Wingate tracks down Siemens funds
by Alex Rozier, Mississippi Today
July 14, 2025
U.S. District Court Judge Henry Wingate said he's putting his decision on hold over whether to approve JXN Water's proposed rate increase until after he finds out what happened with roughly $90 million from a settlement with Siemens.
In 2020, the city of Jackson settled its lawsuit with the German company over years of faulty metering for water services. While about a third of the $90 million went to legal fees, city officials couldn't immediately say where the rest of those funds went during a status conference Monday.
City Attorney Drew Martin said he was working to comply with a subpoena Wingate issued last week looking for an accounting of the settlement dollars, adding that he would have those details within a day or two. While he couldn't say for sure where the money went, Martin said the city spent about $50 million within a few months after the settlement, and that there was $8 million remaining as of 2022.

Ted Henifin, who runs JXN Water and first proposed the rate increase in February, said the increase would still be necessary even if the utility received all the money from the Siemens settlement. He said the utility's day-to-day management is operating at a deficit, and that the $60 million from the settlement — what Jackson received after paying its lawyers — would only cover losses for the next two years.
Henifin added that he's asking the federal government to move around its funding to the city so he can spend more of it on operations and management. Without a boost to JXN Water's finances, he said the utility would have to stop paying its contractors.
Wingate inquired about the settlement money during a two-day status conference last month. Henifin told the judge he had no idea what the city did with the funds. Wingate explained Monday that he wanted to make sure he was aware of all possible funding for JXN Water before approving a second rate increase in as many years.

It's unclear how soon he'll decide. In addition to Jackson officials, Wingate issued the subpoena on July 9 to the state and federal government as well as four different law firms. The subpoena gives the parties 30 days to produce any information on where the settlement funds went.
The judge also brought up the city's history with shutting off nonpaying customers. Martin explained that the city, under then Mayor Tony Yarber, agreed to pause shutoffs for customers who had issues with Siemens' water meters. Jackson prepared to bring back shutoffs in 2019, he said, but put them on hold again during the COVID-19 pandemic.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.

From jailhouse lawyer to clerk of court candidate
Calvin Duncan’s unfinished mission for justice moves to his political candidacy
by Bernard Smith July 15, 2025
For nearly four decades, Calvin Duncan has worked to help incarcerated people get records from the clerk of court office.
When he finally got his own records, he found numerous errors that pointed to his innocence. That led to his release — but not until he’d served more than 28 years in prison.
In a poetic moment on Friday, Duncan officially qualified to run for Clerk of Criminal District Court In Orleans Parish.
Duncan believes that a clerk who truly understands the stakes can reshape how the office operates.
As he stood in front of the courthouse on Tulane Avenue after qualifying for office on Friday, he explained why he was running for the office held by Darren Lombard. “In 1982, I was in prison for a crime I didn’t commit,” he told the gathered crowd. “I always had problems trying to get records from the clerk of court here.”
His campaign is focused on three central goals: ensuring court records are accurate and accessible, making election operations transparent and fair, and turning the clerk’s office into a place of public trust and service.
“I decided today I was going to attempt to make a change by becoming a clerk so that we can help people get access to their records,” said Duncan, who has heard for years about loved ones who got “the run-around” when trying to get records, he said. “Family members that come here should be greeted with respect and dignity. It shouldn’t be a difficult task just to get records.”
Duncan’s name is already well-known to many in the legal-reform community. After his release from Angola State Penitentiary, Louisiana’s infamous maximum-security prison, Duncan is determined to change the system so that no one else faces the wrongful charges based on nonexistent physical evidence and questionable testimony.
That makes Duncan’s campaign for Clerk of Court more than just another political bid, he said. The clerk’s office, often overlooked by voters, plays a vital role in record-keeping, election oversight, and access to court documents.
Duncan filed for office only a few days after Penguin Random House released his memoir, The Jailhouse Lawyer, co-written with Sophie Cull, which tells his story, as a 19-year-old, wrongfully convicted Black man who taught himself the law behind bars, to make up for the failures of the criminal-justice system.
Key to his struggle was his inability to get his records.
The struggles for records are most difficult for anyone who is incarcerated, he said. “Anybody in the world could come to this city to get access to their records other than the people that’s in jail.” He recalled his frustrations with that issue when he was at Angola. “It’s our record and we can’t get access to it.”
Upon his release, won with the help of the Innocent Project New Orleans, Duncan refused to stop. He attended Lewis & Clark Law School in Portland, earned a Juris Doctor degree, co-founded the Light of Justice Initiative. His legal career is marked by his roles in landmark legal victories like Smith v. Cain and Ramos v. Louisiana.
True reform begins with those who know the failures of the system from surviving it, Duncan said.
“From a prison law library to the parish ballot,” Duncan says, “I’ve walked every inch of this journey. Now it’s time to put power where it counts.”
Proposed Public Media Cuts Will Hurt Rural Americans
by Ilana Newman, The Daily Yonder
July 16, 2025
Trump administration funding cuts to public media through a rescissions bill currently moving through Congress would affect rural and tribal areas most, leaving some regions without local reporting and vital community connection.
Alaska’s Yukon-Kuskokwim Delta is a region about the size of the state of Oregon. It’s inaccessible by road. Bush planes, boats, and in the winter, snowmobiles, are the only form of transportation. Here, where the Yukon and Kuskokwim rivers meet the ocean, 58 communities and more than 23,000 residents, most of whom are native, call the tundra home.
KYUK public broadcasting serves the Yukon-Kuskokwim Delta through public radio and television programs and broadcasts bilingually in English and Yup’ik, which many elder residents speak as a first, or only, language.
This Rescissions Act is a Trump Administration agenda bill that would authorize Trump’s funding cuts to public media, if Congress approves it. The bill, which has passed in the House of Representative and is currently in the Senate, would cancel $1.1 billion in already appropriated funding for the Corporation for Public Broadcasting (CPB).
245 of the 544 stations that receive CPB funding are rural, and rural stations depend more on this funding than their urban counterparts. On average, rural stations rely on CBP for 17% of funding and some tribal stations receive more than 50% of their funding through CPB.
“The communities that will be most affected are the ones that are the smallest and have the most to lose. Rural America deserves to be able to be seen and heard through public media,” said Sage Smiley, news director for KYUK.
The Senate has a July 18th deadline to vote on this bill. Democratic Senators are loudly opposed, but even Republican Senators who represent rural communities have expressed apprehension about the proposed cuts.
Susan Collins, Republican Senator from Maine, said in a Senate Appropriations Committee Hearing in June that “in Maine, this funding supports everything from emergency communications in rural areas, to coverage of high school basketball championships and a locally produced high school quiz show.” There are other ways to address the “bias at NPR,” she said, “than rescinding all of the funding for the Corporation for Public Broadcasting”

It’s a similar story in Alaska. Federal funding through CPB makes up 70% of KYUK’s budget. If funding is cut to CPB, KYUK would need to make some major changes, according to Smiley.
“The goal is to keep KYUK on the air and maintain its licensure, which [if the Rescissions Act is passed] would require some incredibly drastic cuts to staff from what I understand,” said Smiley.
Patricia Harrison, President and CEO of the Corporation for Public Broadcasting (CPB) said in a statement that there’s economic value to funding public media. “Federal funding is essential to public media. Every dollar from CPB brings nearly seven more from state, local, and private donors – the kind of return any taxpayer would insist upon.”
“Public broadcasting exists for everyone. It's not pay to play. It's not behind the pay wall,” said Smiley. She added that in her region, many people cannot afford to pay for their news, local or otherwise.
In rural areas like the Yukon-Kuskokwim Delta, local news is not a given. In 2024, the number of news deserts, or counties without any local news, rose to 208. But it’s not just the existence of a news source, its quality also matters. Many small papers have been gutted due to funding cuts, leaving a reporting staff barely able to cover local issues.
Smiley said that in the Yukon-Kuskokwim Delta, the other main source of news for the region is a newspaper that mostly prints press releases and photos. “It does not do the kind of news that KYUK does,” she said.
Studies have shown that without local reporting, government corruption grows. Having local reporters present at county meetings is sometimes the only way residents get updates on local issues. And in many rural areas, federal funding is the only way to support these on-the-ground reporters.
Smiley also said she sees that statewide or national news coverage of her region sometimes lacks nuance and context. “When you're disconnected from community, when you're reporting from elsewhere, you end up missing the mark,” she said.

In Southwest Colorado, KSUT was created in 1976 as a tribal radio station and communication resource for the Southern Ute reservation. The station aired programming mostly in the Ute language with community news and tribal music.
Today, KSUT serves the entire Four Corners area, from the Southern Ute reservation outside of Durango, to Navajo Nation and Jicarilla Apache in New Mexico.
In May, KSUT joined forces with NPR and other Colorado radio stations to sue the Trump Administration over an executive order to end federal funding of public media. This lawsuit argued that because Congress controls funding, an executive order changing the flow of funds without congressional buy-in is unconstitutional. If the Rescissions Act passes, those opposed to public media funding cuts will no longer be able to make this argument.
On reservations many residents don’t have reliable internet access, which makes radio an essential source of connection to their community. “Tribal-serving stations help reach some of the most underserved, under-heard people in the country,” said Tami Graham, KSUT’s executive director.
Radio is one of the best forms of emergency communication for these regions as well. “When you're out on the rez and you have no internet and you're trying to figure out ‘this flash flood, can I cross safely?’ The only way you can get that information is through your local community tribal-serving station,” said Graham.
KSUT receives 20% of their budget or around $330,000 annually from CPB, said Graham. If the Rescissions Act passes, Graham said they will go straight into fundraising mode. KSUT, and many public radio stations, already have a plea for donations on the front page of their websites.
“It'll be terrible but we are going to get through this. I have faith in our communities that we're going to find a path forward,” said Graham.
This article first appeared on The Daily Yonder and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.